Equity issues have always been inherent to public health concerns of society. Questions like who gets what service, who are left out with this intervention and who benefits the most, and how to distribute and allocate limited resources, are some questions that may come to mind when thinking of equity, particularly in the context of an ever-growing landscape of health technologies.
Tackling equity and efficiency is commonly challenging in priority setting decisions, especially for low middle-income countries like the Philippines where both are crucial concerns in decision-making. As appraisal of evidence on the impact to equity of a particular health technology is traditionally conducted outside the analysis of cost-effectiveness, we easily fall to the fallacy of the trade-off between the two, instead of analyzing the evidence altogether that looks at achieving these two. As such, a hurdle to these challenges and questions are the methodologies to answer them systematically and rigorously. Thus, the National University of Singapore’s Distributional Cost-effectiveness Workshop helped us make strides towards answering these questions.
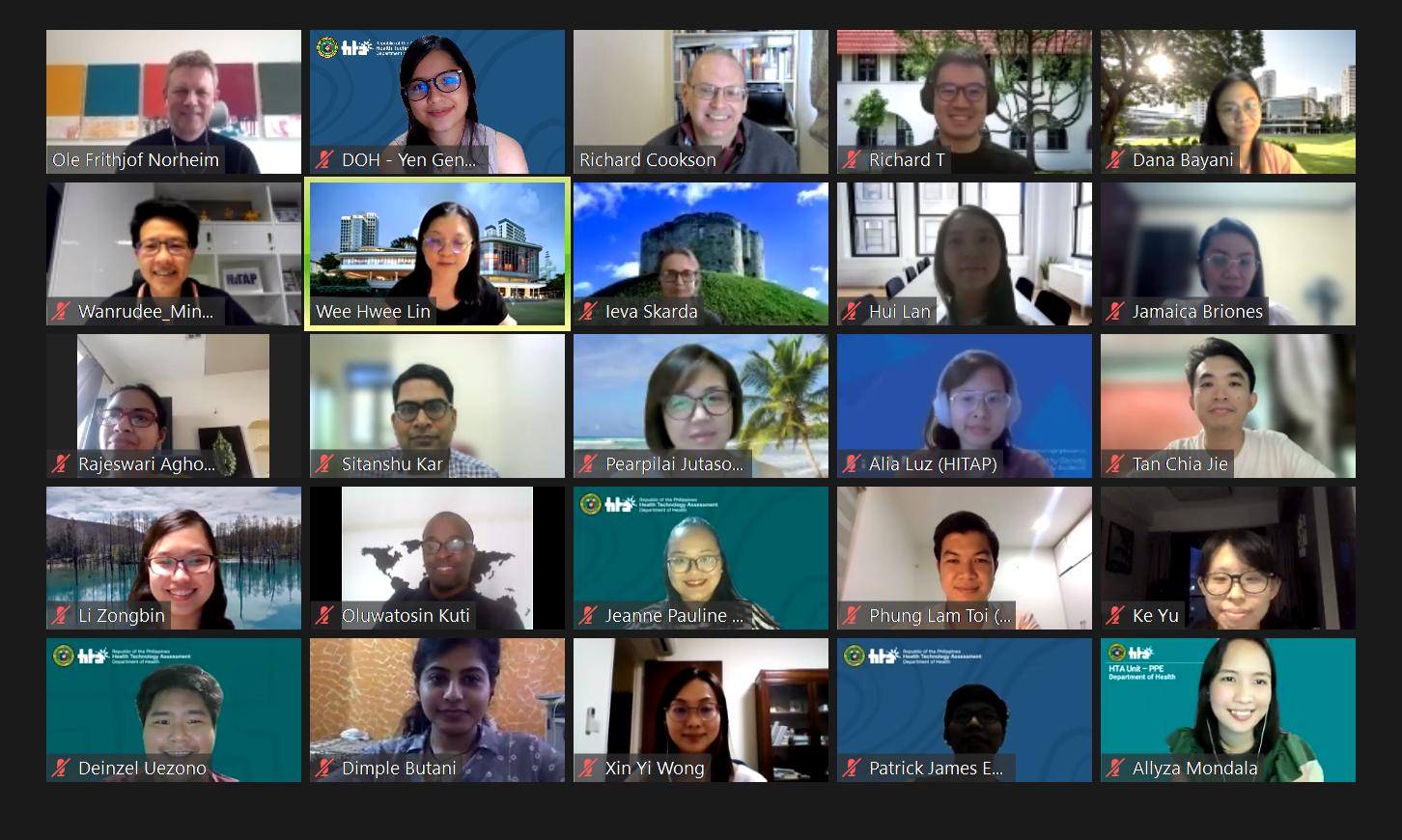
Last April 19-23, we were fortunate enough to have members participate in the NUS Distributional Cost-effectiveness Analysis Workshop. We are honored to have been given the chance to hear from distinguished lecturers who are well respected in the area of HTA, health economics and equity. The course provided us with a solid foundation of the concepts and methods by which we can incorporate equity into cost-effectiveness analysis to aid in decisions for better health outcomes. The course was delivered through a mix of strategies that included lectures, small group discussions, and hands-on exercises to ensure optimal learning despite the limitations due to the pandemic.
Collectively, we found that incorporating equity within the cost-effectiveness analysis means weighing in the different socioeconomic factors and the capacity to use finite resources to the needs of the population. By doing so, weighing in equity significantly affects the total cost such that it may help identify which population will benefit more from the supposed health technology. We learned that there are several measures that can be applied to incorporate equity in economic evaluations such as equity weighting and Atkinson’s inequality measure (aversion to inequality). This information can be very helpful in guiding our decision-makers in allocating resources that takes into account equity within the analysis of efficiency. By having one analysis that incorporates both efficiency and equity, it becomes easier to present to policy-makers in deciding how much more they are willing to spend in order to achieve equity. Overall, we are grateful to have been included and witnessed lectures from well respected experts in HTA.
We recognize the importance of this methodology in our work, to not only look at the traditional efficiency endpoints but also to consider and measure equity parameters in our economic analysis for better health outcomes. After all, as Professor Richard Cookson mentioned in one of his journal articles, what doesn’t get measured gets marginalized.