This essay is written by students from the Philippines who studied a course on health economics conducted by HITAP. HITAP staff assisted in teaching the course and the essays featured on the HITAP website were examination answers submitted by students on the course.
The COVID-19 pandemic has further magnified the cross-cutting global problem on limited resources, especially in low to middle income countries. This has further taken a toll on the healthcare system, as part of the wider economic crisis due to lockdowns imposed in containing the virus. Consequently, since healthcare system resources were concentrated and directed to attend COVID-19 matters, procurement of vital supplies continued to deplete, thereby causing the already limited resources to decrease to the point of shortage.
Since the signing of the UHC Law of Philippines in 2019, the Health Technology Assessment Council (HTAC), together with the Health Technology Assessment Unit (HTAU) in the Philippines have been working tirelessly to assist our decision makers in providing and implementing evidence-based policies in COVID-19 health technology needs, as well as other health systems and healthcare needs. HTA, including health economics, is a very important tool for informed decision making and in aiding policy making and managing finite resources. While there is much to be done for an admittedly young team like ours, there is also much to be learned. With this, HITAP and Mahidol University’s short course on Health Economics truly helped us appreciate and be more effective in doing health technology and economic assessments.
Last May 24 – July 19, 2021, we were fortunate enough to have members participate in the Mahidol University’s elective course: ADPM 613 Health Economics through the generosity of our colleagues in HITAP. We are honored to have been given the chance to hear from distinguished lecturers who are well respected in the area of HTA, and health economics. The course provided us with abundant learnings on the concept and methods of economic evaluation. Due to the limitations in the learning strategies brought by the pandemic, lectures, discussions and hands-on exercises were delivered online. Nevertheless, the course was crafted effectively to ensure fruitful learning for us students. We were able to understand how health technology assessment is being applied at different levels in the health systems and how economic evaluation principles ensure the effective management of limited resources. Also, the course showed us how HTA is applied in the actual setting of policy planning and policy making.
Insights on health economics and HTA topics – Applicability in the Philippines
By the DOH – HTA Unit Philippines
During the ADPM 613 course, several issues, scenarios and topics related to health economics and HTA were also tackled. With the help of our lecturers and participant colleagues from different countries in Asia, we were able to contextualize and further understand the applicability of HTA and health economics to our own setting, with nuances coming from our own health systems experience. The following are some topics discussed throughout the course and our insights on their importance and practical implications in different settings, especially in our country.
1. What is the role of health technology assessment and health economics in the age of pandemics?
Health technology assessment (HTA) is defined as a “multi-disciplinary method to determine the value of a health technology” Its role, especially in time of this pandemic, has become more evident and significant. Since HTA is an evidence-based and flexible process which can be applied at any point after the manufacture of a health technology, it will be an important method to be able to assess the safety and effectiveness of health technologies. Doing HTA during a pandemic would help inform the government’s decisions in line with the vaccination deployment plan and overall response to COVID-19. In the Philippines, health technology assessment is currently playing a huge part in the decision making of the government, especially in determining if the vaccines issued with emergency use authorization by the regulatory agencies are confirmed to respond to disease, magnitude, severity, and equity; safe, efficacious, cost-effective and affordable and would be given a positive recommendation for the continued procurement and use. The involvement of evidence-based reviews on the expedited manufacture of vaccines helps not only the decision makers but also the people to be well-informed of the possible consequences of its use. Currently, all reviews and appraisals made by the HTA Unit are being published on a website to be able to cascade to the public the recommendations of the HTA Council which have undergone fair and transparent processes. The HTA has been one of the aids of the government in its decision making to assure that appropriate health technologies are procured and given to everyone. In this pandemic, health economic assessment helps by determining budgetary impact as well as health benefits a specific type of vaccine could deliver. Moreover, through health economics, the government can prioritize the treatment of a person depending on the severity of the disease giving an equitable chance to every individual.
While HTA provides the recommendation of which health technologies are to be procured, the government is responsible for providing the people with equitable access to quality and affordable health services. This brings us to our next question:
2. Should health insurance services be provided for all by the government?
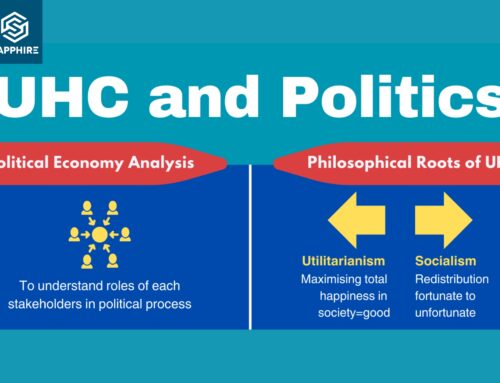
Health, and access to quality health services is a basic human right. The Director-General of the World Health Organization (WHO) once said “The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition”. In 2015, all member states of the United Nations agreed on the Sustainable Development Goals (SDGs). With this, they have set out an ambitious agenda for a safer, fairer, and healthier world by 2030. One of these targets under SDG no. 3 is the achievement of universal health care or UHC. According to the WHO, Universal Health Care (UHC) is about ensuring all people and communities have access to quality health services where and when they need them, without suffering financial hardship. It includes the full spectrum of essential, quality health services, from health promotion to prevention, treatment, rehabilitation, and palliative care across the life course. Therefore, in line with the goals of achieving UHC for a better world, we are in favor of the provision of health insurance for all by the government.
This however, admittedly is a difficult feat to attain for a lower-middle income countries like the Philippines. There have been competing public health and government priorities especially in the age of the COVID-19 pandemic. Based on the 2020 SDG report of the United Nations (UN), the world is falling short on its promise of universal health coverage by 2030.The ideal set up in a perfect world would indeed be free healthcare access for all. However, a better and more attainable goal would be a healthcare and health insurance system that would enable the government to provide equitable access to services and medicines to those who need it. In the 2021 SDG report, improvements in coverage have been reported in all regions and in all income groups. If we can do it despite the pandemic, then imagine the improvements in health coverage that we can achieve when the pandemic officially ends.
Providing insurance for all of your citizens would mean investing in their health and in turn productivity. The more productive citizens are, the more productive the country gets. In the Philippines, where the out-of-pocket health expenditure is around 47.9%, the government strives to lower this and provide equitable access to healthcare through the passing of RA 11223 or the Universal Health Care Law. One provision of the law was to automatically enroll all indigent citizens, senior citizens and persons with disabilities as indirect contributors to the Philippine Health Insurance Corporation (PhilHealth), the national health insurance provider of the country. This would enable the indirect contributors to be covered with health insurance when they need it. Other productive citizens then, as direct contributors, will still continue to pay a premium for their PhilHealth coverage, as a form of social solidarity. Other funding sources for health would be taxes from citizens and the Sin Tax implemented by the Philippines to cigarettes and alcohol among others. In the spirit of fairness and equity which are some of the main agenda of SDG, the UHC Law institutionalized priority setting mechanisms like the HTA that can help us identify core health care services that can be provided in health insurances for all in case the government has limited budget. This has been one of the main strategies of 9 out of 10 countries for the continuity of essential health services as identified by a WHO Survey in the SDG 2021 report.
As aforementioned, UHC is a big endeavor for the government to attain in a short period of time. True health insurance coverage for all is still a bit far for our country, but we are on our way. One thing to be of help would be to improve systems that would manage health funds, and to strengthen research and studies that would generate evidence-based policies that would promote transparency, integrity and efficiency in providing the best healthcare possible to Filipinos.
It was repeatedly stated that resources are limited and proper allocation of these resources is essential in providing the best services to the people. The succeeding topic would elaborate how and why it is important to manage our resources appropriately.
3. Why is it important to have an explicit process and criteria for resource allocation?
There are two (2) ways in which a certain organization or government can prioritize: 1) implicit priority setting and 2) explicit priority setting. Implicit priority-setting is, by the definition of implicit, considered an informal method, possibly ad hoc, where there is no set or explicit system for making decisions. This method may disadvantage the worse or the least well off and possibly interrupt or make the path to UHC distorted. This disadvantage can be addressed by having an explicit priority-setting criterion.
Explicit priority-setting is a mechanism wherein the methods, criteria, and processes are clearly set out and involves various stakeholders. This way of prioritization is driven by a scientific process, where trade-offs between different options can be weighed off before finally deciding on the priority. In developing the criteria, numerous methods can be considered. For example, a Delphi technique where a panel of experts is surveyed. There is also a Discrete Choice Experiment where selected participants, preferably those who represent your stakeholders, are to choose between pre-selected criteria which can be borne out of a review. Another example is the multi-criteria decision analysis where decisions are based on more than one criterion. One example is the Health Technology Assessment (HTA). As defined in the UHC Law of the Philippines, the HTAC must consider the following criteria to guide their recommendations: (1) responsiveness to disease magnitude, severity and equity; (2) safety and effectiveness; (3) household financial impact; (4) cost-effectiveness and (5) affordability and viability.
Transparency and accountability are the most important characteristics that explicit priority setting brings into the table. It ensures that all actors and stakeholders are well-informed and acquainted with the proceedings, have a clear idea of their roles and responsibilities, and are aware of all factors that are considered in the assessment process and exact procedures leading to the final decisions. An explicit process and criteria for resource allocation also ensures that relevant stakeholders can actively participate in the process and undertake necessary actions that are expected of them.
According to a survey by Seixas et al., 2021, there is a widely held understanding that decisions should be based on multiple explicit criteria, to which participants also emphasized that transparency, legitimacy, and fairness of decision frameworks are resource allocation is still largely carried out based on historical patterns and through ad hoc decisions due several barriers such as – vested interests, political resistance, lack of trust among stakeholders, and media pressure.
With the pandemic at hand, one of the major challenges among countries is resource allocation for vaccine procurement. The HTAU examined vaccine procurement among countries as discussed below:
4. What are the advantages and disadvantages of COVAX compared to bilateral agreements with vaccine manufacturers?
The COVID-19 Vaccines Global Access (COVAX) initiative co-led by Coalition for Epidemic Preparedness Innovations (CEPI), the Global Alliance for Vaccines and Immunization (GAVI), and the World Health Organization (WHO), in partnership with the United Nations International Children’s Emergency fund (UNICEF) aims to accelerate the development, manufacturing, and delivery of COVID-19 vaccines to every country in the world. It seeks to guarantee equal access to the vaccines for every country in the world. The COVAX offers a diverse and actively managed profile of vaccine doses for at least 20% of a country’s population, as well as immediate vaccine delivery the moment they are available with the goal of ending the critical phase of the pandemic and rebuilding economies.
One of the advantages of participating in the COVAX initiative is that in essence, it is a form of bulk-purchasing strategy to avail the needed COVID-19 vaccines at a relatively lower cost through economies of scale. This enables small and middle income countries, such as the Philippines, to have access to these successful vaccines equitably through the facility who negotiates with the vaccine manufacturers for them. By negotiating with various vaccine manufacturers, it has a wide portfolio of vaccines which ensures that a member country will end up with a supply of successful vaccines once available. The issue of price may also be an advantage for the COVAX facility because for countries that otherwise might not have the budget to purchase the amount of vaccines they need, they will be able to purchase because of the pooled funds and price negotiations of the initiative. This further gives those countries the opportunity to get vaccines within their budget or may be lower than their allocated fund. It would definitely be a win-win situation for all the countries. Furthermore, through COVAX, it is assured that vaccines will consistently be of quality. it will also guarantee equitable access and affordable prices for all countries. Lastly, one of the best advantages as well is that it would already cover logistical costs; thus, it will be delivered safely to a country without incurring additional cost since the excess allocated budget may be used to pay for the logistical costs. Add statements on disadvantages of COVAX such as slow movement of supplies.
If a country chooses a bilateral agreement method to procure a vaccine, that country may incur more cost than through bulk purchasing through COVAX. We are aware that all countries have a different allocation and budget for the vaccine procurement however, the manufacturers would not base their pricing on a country’s fund thus, a baseline price is given by the manufacturer; in that case some countries may afford the procurement price and some won’t. Furthermore, price negotiation may be hard if a country purchases through bilateral agreement since only a lower quantity or amount will be purchased, it would be hard to negotiate with the price. Lastly, a disadvantage is that additional logistical cost may be required and the specific country may need another set of budget just to cover delivery/transportation and storage costs. Moreover, wealthier countries may exploit the bilateral agreements while procuring quality vaccines ahead of other countries. This will in turn result in these countries being prioritized by the companies over the facility causing delay in deliveries and availability for COVAX. This is what is happening right now, as the line for vaccine delivery is already long, and wealthy nations are already almost to their target vaccination percentages, while small nations are only starting their rollout.
In the end, a thorough assessment of the country’s situation should be done to decide on what route to take, whether to join the COVAX initiative or not, and do bilateral agreements.
5. What are the ways that a government can negotiate or manage the price to facilitate the inclusion of a technology in the benefits package?
The government can negotiate or manage the price of health technologies to facilities package inclusions in several ways. One example is policy-driven negotiation by ‘value based pricing’ using HTA. In this method, evidence from economic evaluations (EE) are used to support government negotiations ultimately deciding on whether to include or exclude health technologies in the benefit package. HTA-generated evidence can facilitate price negotiations by simply informing stakeholders, especially market suppliers on the relevant EE results – incremental cost-effectiveness ratio (ICER) values and thresholds which supports the coverage decision of a particular health technology. This was the case with Oxiplatin and 3-dose HPV vaccines in Thailand which initially concluded as ‘not cost-effective’. Through price negotiations Oxaliplatin price was reduced and ultimately included in the National List of Essential Medicines (NLEM) in Thailand. Meanwhile, pharmaceutical companies eventually reduced the price of HPV vaccines by 60% following the results of the economic evaluations conducted. While the government chose to focus their budget on screening efforts, the general public still benefited from its reduced sale price.
Another way to negotiate the price of health technologies is through ‘managed entry agreements’ usually associated with expensive, innovative therapies. One example of managed entry agreement is the price negotiation of ‘codependent technologies’ with suppliers such as in the case of Trastuzumab and FISH test. Another example is thru ‘risk sharing agreement’ used to address uncertainty about the performance of technologies or to manage the adoption of technologies in order to maximize effective their use, or limit their budget impact. This model was used in the case of Imiglucerase inclusion in the Thailand NLEM. The government agreed to pay the full price for the first five years of treatment of imiglucerase, while on the other hand the supplier agreed to reduce the price by 46% in the following years of treatment.
Third example is the use of ‘compulsory licensing’ which allows a government to produce or import a generic medicine without consent of the patent holder for a limited period of time. In this method, the patent holder still receives compensation in the form of a royalty (usually a percentage of drug price). Thailand has used this mechanism in some anticancer drugs including Letrozole and Docetaxel to overcome the cost barrier of access to drugs through the more affordable generic equivalents (Mohara et al., 2012).
In the Philippines, we have a Price Negotiation Board (PNB) which was created under the UHC Law. The PNB is an independent body that negotiates prices, on behalf of the DOH and PhilHealth, to assure that the best negotiated price is achieved. The negotiated price would guarantee that the most affordable yet quality health products will be provided to the people.
Finally, as our team is still in the early stage of exploring the use of health economics in our country, we are confident that the HITAP and Mahidol University’s short course provided us with a solid foundation in the appreciation of health economic assessments.
References:
GAVI, The Vaccine Alliance (2021) COVAX Explained. Retrieved July 21, 2021 from: https://www.gavi.org/vaccineswork/covax-explained
Ghebreyesus, T.A. (2017). Human Rights Day 2017 Message. Retrieved from https://www.who.int/news-room/commentaries/detail/health-is-a-fundamental-human-right
HITAP Lecture Slides
HTA Philippines (2021) HTA AND THE COVID-19 PANDEMIC. Retrieved July 21, 2021 from: https://hta.doh.gov.ph/2020/10/02/hta-and-the-covid-19-pandemic/
HTA Philippines (2020) Philippine HTA Process Guide. Retrieved July 21, 2021 from: https://drive.google.com/file/d/1yJI8_D5VgKbp8mGkKJUNH39vzbBiVuZf/view
Mohara, A., Yamabhai, I., Chaisiri, K., Tantivess, S., & Teerawattananon, Y. (2012). Impact of the Introduction of Government Use Licenses on the Drug Expenditure on Seven Medicines in Thailand. Value in Health, 15(1), S95–S99. doi:10.1016/j.jval.2011.11.016
PhilHealth. Ano ang Universal Health Care o UHC?. Retrieved from https://www.philhealth.gov.ph/uhc/
Seixas, B.V., Regier, D.A., Bryan, S. et al. Describing practices of priority setting and resource allocation in publicly funded health care systems of high-income countries. BMC Health Serv Res 21, 90 (2021). https://doi.org/10.1186/s12913-021-06078-z
United Nations (2020) SDG Report 2020. Retrieved July 21, 2021 from: https://unstats.un.org/sdgs/report/2020/goal-03/
United Nations (2021) SDG Report 2021. Retrieved July 21, 2021 from: https://unstats.un.org/sdgs/report/2021/goal-03/
WHO (2021) Universal Health Coverage. Retrieved July 21, 2021 from: https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc)